Warning: TIA can lead to a stroke
Last Friday, Oct. 10, I was having dinner with some of my son’s friends and their parents when in the middle of our meal, I noticed that the mother of his friend kept leaning toward her left side. Each time, she straightened up again without any effort, so I didn’t think much of it. After dinner, we took a short walk to a nearby frozen yogurt stall. Everyone ordered their favorite flavors and toppings, and we were laughing and chatting when suddenly, Elaine (let’s call her that) started to lose her balance. Her left knee began to wobble, and she said she felt a strange sensation running down her left forearm.
Somehow, she managed not to drop her ice cream—which we all joked about later—but we quickly sat her down to rest. When it was time to go, I noticed something wasn’t quite right. Her walk had changed—she was moving slowly and seemed to drag her left leg a little.

The next day, I couldn’t shake the worry, so I called to check on her. She told me it felt like she was dragging three pails of water tied around her waist. Thankfully, there were no other alarming symptoms—no slurred speech, drooping face, vision problems, or confusion.
By that evening, though, she still wasn’t feeling better, so I advised her to go to the ER. The doctors ran several tests and recommended that she be admitted to the ASU (Acute Stroke Unit) for observation and bed rest. Thankfully, her condition continued to improve. Aside from a slight balance issue, she was back to her usual self. By 8 p.m. that night, she was discharged—with a diagnosis of TIA (Transient Ischemic Attack) and some take-home medications. It was a huge relief, but also a wake-up call.
What is transient ischemic attack?
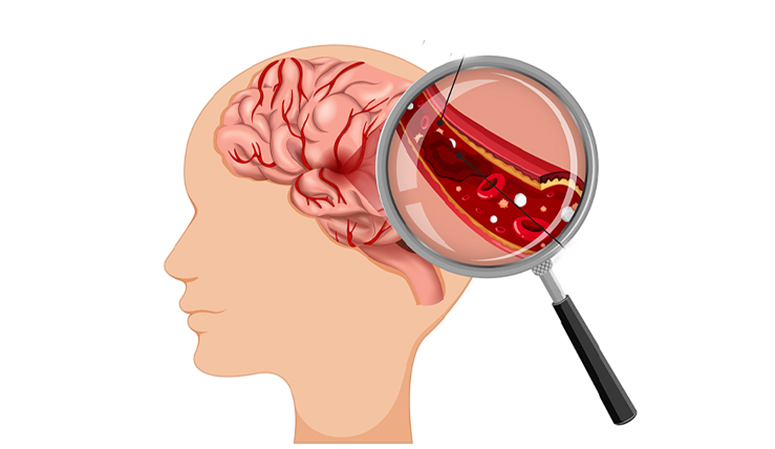
A transient ischemic attack is like a temporary stroke, where there’s a temporary (transient) lack of blood flow to a part of the brain. Without blood flow, the brain cells malfunction and start to die (ischemia).
Often shortened to TIA, a transient ischemic attack is a medical emergency that’s very similar to an ischemic stroke. The symptoms of the two are the same, but TIA symptoms may go away within 24 hours (most go away in minutes). However, there’s no way to predict how long a TIA will last, and every minute counts. Seek immediate medical help if you have signs, including balance issues, vision changes, face and arm drooping, and speech difficulties.
Don’t wait to see if the symptoms will subside, and call for help even if the symptoms get better after a few minutes of resting. A TIA can be the precursor to a stroke, so get medical attention right away!
TIA vs. mini-stroke—which is the correct name?
A common nickname for TIAs is “mini-strokes.” But that’s not an accurate name. A TIA isn’t necessarily “mini” or smaller, and TIAs can easily affect large brain areas. Importantly, a stroke may occur after a TIA, within a matter of minutes, hours, or days.
There are also two critical differences between strokes and TIAs. The first is that a TIA stops on its own. A stroke doesn’t, and it needs treatment to stop and reverse the effects. A stroke also leaves behind evidence on a magnetic resonance imaging (MRI) scan. The changes remain even if your symptoms go away.

TIA symptoms
The possible symptoms of a TIA are nearly identical to the possible symptoms of a stroke.
The symptoms of an ischemic stroke can involve one or more of the following: one-sided weakness or paralysis (hemiplegia); difficulty with or loss of speaking ability (aphasia); slurred or garbled speech (dysarthria); loss of muscle control on one side of the face or facial droop; sudden loss—either partial or total—of one or more senses (vision, hearing, smell, taste and touch); blurred or double vision (diplopia); loss of coordination or clumsiness (ataxia); dizziness or vertigo; nausea and vomiting; neck stiffness; emotional instability and personality changes; confusion or agitation; memory loss (amnesia); headaches (usually sudden and severe); passing out or fainting.
Causes
Transient ischemic attacks and ischemic strokes happen for the same reasons, which include: formation of a clot in the brain (thrombosis); a fragment of a clot forming elsewhere in the body that breaks free and travels through the blood vessels until it gets stuck in the brain (thromboembolism); small vessel blockage (lacunar stroke); cryptogenic TIA (the word “cryptogenic” means “hidden origin,” so these are TIAs that happen with an unknown cause).
Risk factors
Many factors can contribute to a TIA or make one more likely to happen. Risk factors include: high blood pressure (hypertension, the most significant of all risk factors for TIA and the reason why managing blood pressure is so essential); Type 2 diabetes; tobacco use (smoking or vaping); Atrial fibrillation (Afib, a heart rhythm [arrhythmia] that can cause blood to swirl and pool in one of the heart’s chambers rather than smoothly flow through. That can allow clots to form, which can then travel through the carotid arteries and into the brain); a history of stroke or TIA. Having a previous stroke or TIA raises the risk of having a TIA.
The main reason a TIA is a medical emergency is that it’s often a warning that a stroke is possible or even imminent. Up to 20 percent of people who have a TIA have a stroke within 90 days, and half of these strokes happen within the first two days after a TIA.
Treatment
A TIA, by definition, is a temporary issue. But it indicates that a stroke—which isn’t temporary—could happen. That means treating the condition(s) that caused the TIA can help prevent a stroke.
Healthcare providers often recommend treating these conditions aggressively. That’s because a stroke is a much more serious—and dangerous—condition. Strokes are also often more difficult to treat. It’s also because even with treatment, strokes can cause permanent damage or death.
A TIA is often called a “mini-stroke,” and while the symptoms can pass quickly, it’s a serious warning sign.


