The truth about the new weight-loss drugs
Comedienne Amy Schumer has tried it. Khloe Kardashian has denied using it. Rosie O’Donnell said it helped her lose 10 pounds. Boris Johnson said he stopped taking it because it made him feel ill.
“It” is Ozempic, an injectable drug used to treat Type 2 diabetics, but it became a TikTok phenomenon when users noticed one of the side effects was rapid weight loss. On TikTok, the hashtag #Ozempic has over 600 million views and counting, and it’s been touted as the new wonder and miracle diet drug.
When he hosted the 2023 Oscar awards, host Jimmy Kimmel joked, “Everybody looks so great. When I look around this room, I can’t help but wonder, ‘Is Ozempic right for me?’”

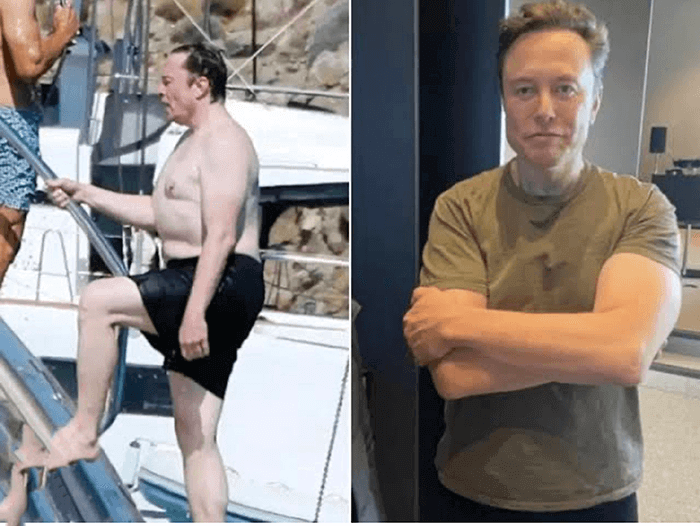
Elon Musk, responding to a tweet asking him about the secret to his physique, credited Ozempic, as well as Wegovy, a similar Semaglutide drug used to treat chronic obesity, as one of the reasons he lost 13 kg: “Fasting + Ozempic/Wegovy + no tasty food near me,” tweeted the Tesla/Twitter CEO.
Hollywood stars who’ve spoken about it include comedienne Chelsea Handler, who said she unknowingly took the medication, claiming her anti-aging doctor prescribed her a drug that was good to use if she wanted to “drop five pounds.” She didn’t know his prescription for Semaglutide was Ozempic until a friend told her. “I’m not on it anymore,” Handler says. “That’s too irresponsible. I’m not going to take a diabetic drug.”
Ozempic’s off-label use for weight loss indeed became a health concern worldwide when skyrocketing demand for the drug caused a shortage for diabetic patients in the United States, the UK, Australia, and France. Authorities called on doctors to avoid prescribing Ozempic for non-diabetic obese patients, and consider alternatives to Semaglutide.
First of all, what is Semaglutide and how does it work? According to doctors, Semaglutide and other glutides mimic a hormone called glucagon-like peptide-1 (GLP-1), which targets the areas of the brain that regulate appetite and food. It makes users feel full faster, and can lead them to lose weight.

However, “potentially serious” side effects include gastrointestinal disorders (severe constipation), pancreatitis (inflammation of the pancreas) and low blood sugar. “In rare cases, it can lead to cancer,” said a French pharmacologist. The US National Library of Medicine warns that it “may increase the risk that you will develop tumors of the thyroid gland, including medullary thyroid carcinoma (MTC), which is a type of thyroid cancer. Lab animals that were given Semaglutide developed tumors, but it is not known if Ozempic increases the risk of tumors in humans.

Dermatologists have also noticed a side effect called “Ozempic face,” in which the face drops like an empty balloon because of the rapid fat loss, so patients have to get fillers to replace lost volume. One derma’s patient got Stevens-Johnson syndrome, a severe drug reaction where the skin blisters and starts to peel off.
As a result, Ozempic manufacturer Novo Nordisk stated it “does not promote or endorse off-label use” of its products—while still investing $1.6 billion in 2022 to expand its production capacity and catch up with demand.

Alternative weight-loss drugs
The drug maker has created alternative drugs like Wegovy (Semaglutide) and Saxenda (Liraglutide) for weight loss in non-diabetics.
Wegovy is used for chronic weight management in overweight or obese adults with at least one related condition, such as Type 2 diabetes, high blood pressure, or high cholesterol.

Marketing for the drug in the US carries warnings for “pancreatitis, gallbladder problems (including gallstones), low blood sugar, acute kidney injury, diabetic retinopathy (damage to the eye’s retina), increased heart rate, and suicidal behavior or thinking.”
Saxenda, meanwhile, is an injectable solution in a pre-filled pen specifically aimed at weight management in obese or overweight adult patients with a Body Mass Index (BMI) of 30 to 40 kg/m2 and the presence of at least one weight-related comorbidity, like dysglycemia (pre-diabetes or Type 2 diabetes mellitus), hypertension, dyslipidemia or obstructive sleep apnea. While Ozempic is injected once a week, you have to inject Saxenda every day to get results.
You want to get on good habits, so use it to get good habits. Like, use it to strengthen your plant-based diet, use it to strengthen your OMAD (one meal a day), or your intermittent fasting, or your Mediterranean diet. Whatever diet you’re on, it will help you stay on that diet, and that way you build up healthy habits. And if, when you're on it, you exercise, you just get into a good lifestyle.
ZP, a healthcare professional, had tried diets, fasting and workouts to lose weight, but once she reached menopause, she noticed the weight wouldn’t come off, no matter what she did.
“I was feeling super-fat,” she says. “I wasn't losing weight on menopause, even with intermittent fasting, doing hard workouts, like, two or three times a week with an hour of weights. Nothing was moving. I was just gaining weight and feeling bloated.”
So she got her doctor to prescribe her a weight-loss drug, which was called Saxenda. “It's by prescription,” she says. “You need to have a doctor, so you can get it either from an endocrinologist or dermatologist.”
First, they gave her a workup, checking her cholesterol, liver, and thyroid, “because there have been reports of pancreatitis,” she says. “If you have a lot of medications on board, you get a basic workup before you start it.”
ZP also attended a webinar about Saxenda, “and they said 5% of your weight in, like, two to three months. Some people starting losing weight in the first two to four weeks after starting treatment. In studies, significant weight loss of at least 5% was seen after eight weeks of treatment. After one year of treatment in adults, 85% of patients treated with Saxenda lost weight (an average of 21 lbs. [9.5 kg] weight loss, or 9.2% of their weight). Your results may be different.
“It sounded good to me and it's pretty safe, generally,” she continues. “So I just had to go for it. This is a GLP-1 receptor so it works on your brain, your muscles, your fat, and it sends signals to your brain that you're full. It doesn't speed up your metabolism, but it makes you lose your appetite. It makes you feel full; it also slows down your gastric emptying time.
“So let's say I eat a meal now,” she relates. “I'll be full until tomorrow if I'm on that medicine. If I'm not on it, I'll feel hungry every three or four hours, right? So this one, I'm fine with one meal a day. So my keto will be super-easy on these medications.”
The most common side effect, she noticed, is nausea. “In my first week, wow, the nausea was intense. I would look at a cheeseburger and want to vomit. You eat a couple of fries and you want to throw up. Oily foods just make you sick. And then you'd be craving a salad; you’re like, I wish I had some cucumber right now. That's amazing. It really does work on your brain.”
Saxenda starts with a low dose of 0.6 mg once daily, which is gradually increased to 3 mg once daily with one-week intervals to improve gastrointestinal tolerability.
Instructions say, “The drug is administered once daily, independent of meals. It should be injected in the abdomen, thigh, or upper arm. The injection site and timing can be changed without dose adjustment. However, it is preferable at Saxenda is injected around the same time of the day. Saxenda should not be mixed with other injectables (e.g. insulin).”
ZP gives herself a shot at night, “anywhere that's kind of fatty. There's a bit of training involved, but there's a training video and your doctor can do the first shot with you. The needle’s tiny; you can barely feel it. There can be some injection reactions like swelling, little hardness, a little bit of itching, some redness—generally it's very tolerable.”
After a month of using Saxenda, ZP has lost only a pound or two, “but my clothes got a lot looser, like, over two, three weeks,” she observes. “And then I measured myself. I lost, like, a cm on my chest and my waist. So you won't lose weight, but this tends to work on visceral fat, which is the fat inside your body and not the subcutaneous fat. If you really want to lose both, do diet, do exercise, eat healthy, no carbs, but it really works more on the visceral fat.”
Treatment with Saxenda should be discontinued after 12 weeks, and its maker, Novo Nordisk, says it’s up to doctors to choose the best treatment approach for their patients.
“You will follow up with your doctor within at least 16 weeks after starting Saxenda to see if it’s working well for you,” ZP says. “If you have not lost at least 4% of your body weight at this time, your doctor may tell you to stop taking it. Even though patients may be doing everything they are supposed to, not everyone will lose enough weight on Saxenda to be able to stay on treatment.”
Other drug companies like Eli Lilly have manufactured competing drugs like Tirzepatide under the brand name Mounjaro for weight loss. Another drug is called Trulicity (Dulaglutide), but it’s a Type 2 diabetes drug that is not FDA-approved for weight loss.
These drug companies say that when accompanied by a comprehensive lifestyle modification program, including diet, exercise and healthy food choices, weight loss of 5% or more has been shown to have a clinically meaningful impact on blood pressure, cholesterol, and triglyceride levels. Otherwise, it’s common to regain the weight (and possibly more if the person binge-eats) after stopping treatment.
“You want to get on good habits, so use it to get good habits,” ZP says. “Like, use it to strengthen your plant-based diet, use it to strengthen your OMAD (one meal a day), or your intermittent fasting, or your Mediterranean diet. Whatever diet you’re on, it will help you stay on that diet, and that way you build up healthy habits. And if, when you're on it, you exercise, you just get into a good lifestyle.”


