When someone you love tells you he has HIV
Two years ago, I experienced one of the most challenging episodes of my life. I had just arrived home from work when the son of a close friend called me, saying he urgently needed to talk to me. I had not seen him in a while, so when he arrived at my house, I was shocked at his appearance. He looked extremely emaciated, with a deeply worried and devastated expression. Even before he could say a word, I feared the worst.
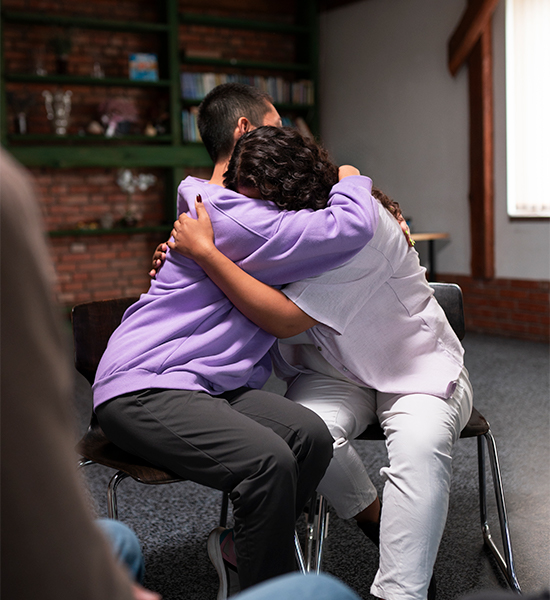
This young man was like a son to me. The moment he broke down in tears, I instinctively told him, “HIV is not a death sentence.” He was surprised that I seemed to already know. I explained that back in 1986, when I worked as a physiotherapist in the US, I cared for many HIV-positive and AIDS patients. I assured him he was not alone in his struggle—cases like his have become more common in recent years.
I asked him if his parents knew. He said no, he was not brave enough to tell them. He admitted he felt completely lost and had even contemplated suicide.
I did my best to comfort him. I assured him HIV was no longer a death sentence and that he could live a full life with proper treatment. I also reminded him that acquiring HIV was not his fault. He wasn’t even promiscuous. Though he was gay, he was shy, conservative, and had only been in three relationships.
His parents were close friends of mine, and I did not know how to break the news to them. At the same time, I knew he needed urgent medical attention. Eventually, I arranged a meeting with his parents and, with great difficulty, found the strength to tell them. Let us call him JR.
Their reaction was immediate—shock, anger, and disbelief. They were furious with him. I gently told them that their response could cause more harm than good, especially since JR was already considering ending his life. I explained the importance of showing love, support, and urgency in getting him treated. Gradually, they began to understand, but it was not easy. As a parent myself, I could sense their fear, sadness, and frustration. It was a truly agonizing experience for everyone involved.
When someone close to you admits to having acquired HIV, it is a significant event that can trigger a range of emotions and reactions. It is important to acknowledge their vulnerability, show empathy, and offer support. While it's not unusual to experience emotional distress or confusion, it's also crucial to understand that HIV is a manageable condition with effective treatments and that people living with HIV can live long and healthy lives.

HIV (Human Immunodeficiency Virus) is a virus that attacks the body's immune system, specifically targeting certain white blood cells called CD4 cells. These cells help the body fight off infections and illnesses. This virus destroys these white blood cells, weakening the immune system and making a person more susceptible to infections, diseases and certain cancers. Our white blood cells will try to fight and slaughter the virus but once overwhelmed by the virus (virus replicating), the virus can eventually destroy these CD4 cells until there will not be enough CD4 cells to fight it. If HIV is not treated, it can progress to AIDS (Acquired Immunodeficiency Syndrome), which is the most advanced stage of HIV infection, and is characterized by a severely weakened immune system. HIV is spread through certain bodily fluids which include blood, semen, vaginal fluids, and breast milk.
HIV can be controlled with medication: Antiretroviral medications can suppress the virus and allow people with HIV to live long, healthy lives.
Symptoms and signs usually involve the skin, the reason dermatologists play a key role in the diagnosis. These range from cutaneous infections to skin cancers and even eczema, very pruritic skin rash that seems trivial and looks like an ordinary skin rash.

It is especially important to inform people that HIV infection can be prevented through PrEP and PEP. Both Pre-Exposure Prophylaxis (PrEP) and Post-Exposure Prophylaxis (PEP) are highly effective in preventing HIV infection when taken correctly and consistently.
PrEP is the medicine people at risk for HIV take to prevent getting HIV from sex or injection drug use. PrEP can stop HIV from taking hold and spreading throughout the body.
Currently, there are two FDA-approved daily oral medications for PrEP. A long-acting injectable form of PrEP has also been approved by the FDA.
PrEP reduces the risk of getting HIV from sex by about 99% when taken as prescribed. Among people who inject drugs, it reduces the risk by at least 74 percent when taken as prescribed. PrEP is much less effective when it isn't taken consistently.
PEP, on the other hand, refers to the use of HIV medicines to prevent HIV infection within 72 hours (three days) after a possible exposure.
PEP should be used only in emergency situations and is not meant for regular use by people who may be exposed to HIV frequently. PEP is not intended to replace the regular use of other HIV prevention methods, such as consistent and proper use of condoms during sex or PrEP.
PrEP is different from PEP in that people at risk for HIV take a specific HIV medicine daily or an injection every two months to prevent getting HIV before an exposure occurs.
The CDC provides guidelines on recommended HIV medicines for PEP. The CDC guidelines include recommendations for specific groups of people, including adults and adolescents, children, pregnant women, and people with kidney problems.
PEP is effective in preventing HIV when it is taken correctly, but it is not 100% effective. The exact effectiveness of PEP is difficult to measure, but observational research suggests that PEP can reduce the risk of getting HIV by more than 80%.


